venous leg ulcer
Das Ulcus cruris venosum ist eine chronische Wunde und tritt meist am Unterschenkel auf, weshalb sie auch als Unterschenkelgeschwür oder umgangssprachlich als “offenes Bein” bezeichnet wird.

The cause of a venous leg ulcer (Ulcus cruris venosum) is an underlying venous disease, such as chronic venous insufficiency, varicose veins, or a post-thrombotic syndrome.
Causes of venous leg ulcers
In a healthy venous system, veins transport oxygen-depleted blood against gravity back to the heart, where it is reoxygenated.
If a manifest venous disease, such as varicose veins, is present, it can lead to ambulatory venous hypertension, resulting in increased venous pressure in the lower legs, ankles, and feet.
The tissue (skin, subcutaneous fat, and connective tissue) is no longer properly supplied with blood, the microcirculation is impaired, and capillary pressure is elevated. This leads to local hypoxia (oxygen deficiency), which can eventually result in the development of an open wound.
A venous leg ulcer can be associated with severe pain and mobility limitations, significantly reducing the quality of life.
In principle, a leg ulcer can have various causes, is often accompanied by severe pain and mobility limitations, and significantly reduces the quality of life.
What is chronic venous insufficiency (CVI)?
Chronic venous insufficiency (CVI) can have the following causes:
Venous Hypertension: Increased pressure in the veins prevents blood from flowing properly back to the heart. This leads to blood stagnation in the legs and increased pressure in the veins.
Venous Valve Insufficiency: The venous valves, which normally prevent the backflow of blood toward the feet, may be weakened or damaged. As a result, blood can no longer efficiently flow toward the heart and accumulates in the leg veins.
Inflammation: Inflammatory processes can damage the vein walls, impairing venous function.
To classify chronic venous insufficiency and treat it according to guidelines, we use the CEAP classification at veins.berlin.
The Leg Ulcer in Connection with Other Diseases
In principle, a leg ulcer can have various causes. For example, it can also develop due to arterial occlusive disease, rheumatological or dermatological conditions, lymphedema, trauma, or diabetes mellitus.
Older adults are particularly at risk for a leg ulcer.
Prevention through regular vascular check-ups of the legs is important.
If you suffer from a leg ulcer or a chronic skin condition in the leg area, timely diagnosis through ultrasound examination and therapy is recommended.
It should also be noted that the treatment of a venous leg ulcer can often be prolonged and requires regular monitoring and individualized adjustment of the treatment by a specialist, along with close home wound management. For this reason, prevention is essential.
How is the treatment of venous leg ulcers performed?
Compression Therapy
Wearing custom-fitted compression stockings or bandages, or a specially prescribed medical-adaptive compression system (MAK), increases pressure on the tissue and veins to improve blood flow and reduce edema (fluid retention). This reduces local venous hypertension and tissue pressure, promoting wound healing and decreasing the risk of further ulcers.
Local Wound Treatment
Proper and individualized wound management is essential to avoid or treat infections and support healing. This may include regular dressing changes, wound cleaning, and the use of special wound dressings or ointments. Wound treatment is usually monitored and performed on an outpatient basis by a trained professional.
Medication Therapy
In some cases, it may be appropriate to prescribe medications such as anti-inflammatory drugs or, in the case of an infection, antibiotics, to reduce inflammation and pain, and treat infections.
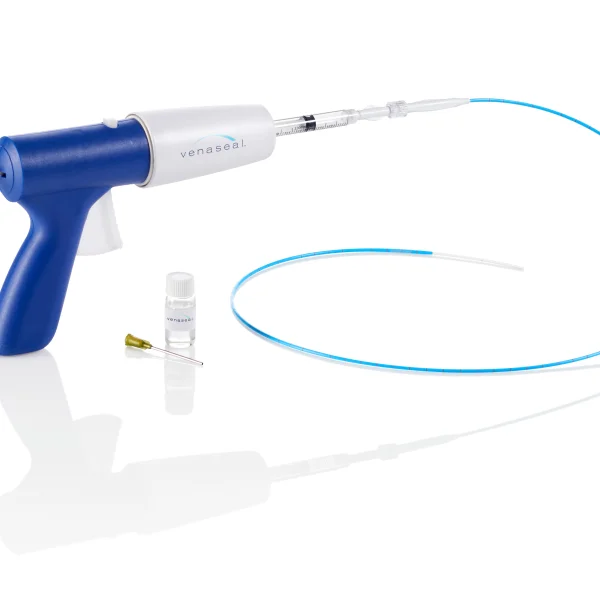
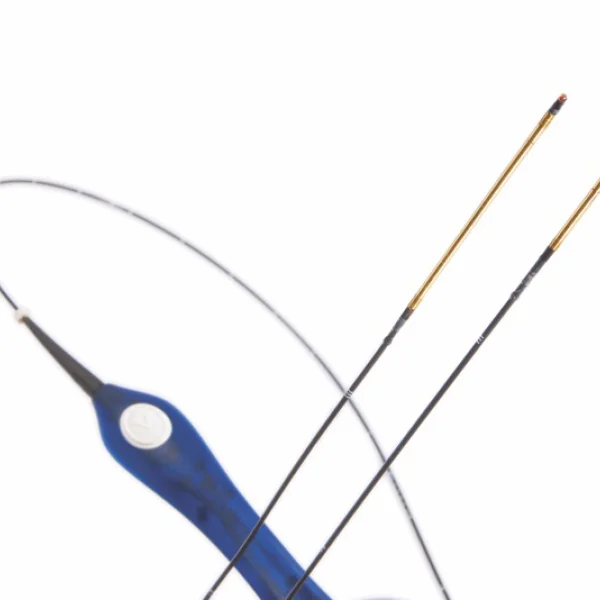
Phlebological/Chirurgical Interventions
In principle, it is advisable to also treat the underlying venous disease, if possible, through an intervention on the venous system. In many cases, this can be done through minimally invasive microfoam sclerotherapy for varicose veins and insufficient perforator veins. Treating trunk vein insufficiency through a minimally invasive catheter procedure or surgical removal of varicose veins is also often beneficial. For large-scale ulcerations, surgical wound cleaning may facilitate faster healing. In rare cases, skin grafts are performed to cover defects in non-healing wounds.