Thrombosis
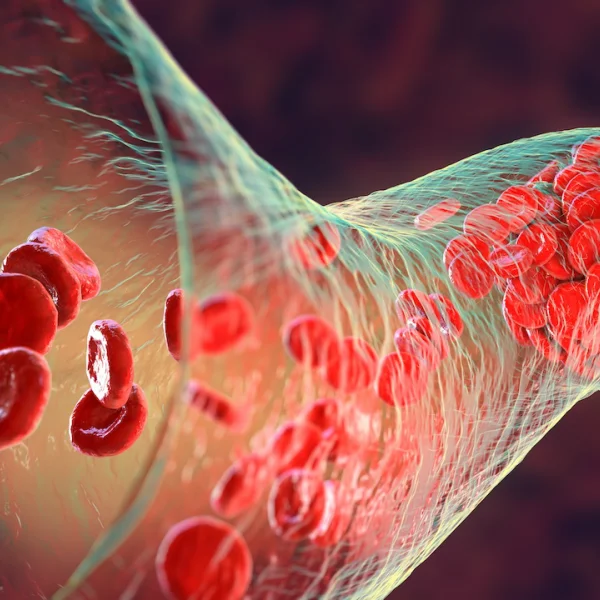
In thrombosis, a blood clot (thrombus) forms in a vein or artery, obstructing blood flow or blocking the vessel.

A thrombosis is a medical emergency.
A thrombosis can theoretically occur in any blood vessel in the body, with varying consequences. If the clot blocks an artery, it is called an arterial thrombosis. This can be the cause of a heart attack, stroke, or acute arterial occlusion in the leg. Blood clots can also form in the heart.
Thromboses can also occur in veins (venous thrombosis). This can happen in various parts of the body, such as in the veins of the brain (for example, as a sinus vein thrombosis), or in the portal vein, which carries blood from the intestines to the liver (portal vein thrombosis). They can also occur in the arm and shoulder vein system (Paget-Schroetter syndrome). A painful anal vein thrombosis can occur around the anus.
A thrombosis can progress acutely, subacutely, or silently.
For clarity, we distinguish in this chapter between:
Superficial venous thrombosis
Deep venous thrombosis
Muscle venous thrombosis
Superficial vein thrombosis is a non-infectious inflammation in the superficial veins, triggered by a blood clot (thrombus) in the affected vein or varicose vein.
What are the symptoms of a superficial vein thrombosis (SVT)?
The SVT typically manifests as redness and palpable, cord-like or spherical hardenings in the affected veins. Strong local pain and a feeling of pressure often occur.
In about 30% of cases, there is also a deep vein thrombosis present, which is a life-threatening condition.
Any suspicion of a superficial vein thrombosis should be promptly evaluated and treated by a specialist, including an ultrasound examination.
In the past, superficial vein thrombosis was referred to as thrombophlebitis.
How does a superficial vein thrombosis develop?
A thrombus forms due to slowed blood flow, blood turbulence, or injury to the vein wall, or dysfunction of the vein valves in varicose veins.
Superficial vein thromboses most commonly occur between the ages of 50 and 70 in the side branch varices, but they can also affect significantly younger individuals.
With increasing age and the duration of varicose vein disease, the likelihood of developing a superficial vein thrombosis rises.
The treatment of a thrombosis, whether deep or superficial, should definitely be carried out and supervised by a specialist.
Diagnosis and treatment of a superficial vein thrombosis (SVT) at veins.berlin
The diagnosis of a superficial vein thrombosis is made through a clinical examination combined with a careful ultrasound examination and your individual medical history.
The treatment of an SVT depends on the location and extent of the formed thrombus and the affected vein segment.
Compression therapy should be immediately initiated through a compression bandage or an appropriate compression stocking. Compression therapy relieves pain and discomfort, helps break down the thrombus by applying external pressure, and normalizes blood flow in the veins.
In the case of pronounced superficial vein thromboses, temporary medication therapy to inhibit blood clotting may be necessary to prevent the thrombosis from progressing into the deep venous system.
Local treatment of the affected areas through cooling, ointments (e.g., heparin), and anti-inflammatory pain relievers can also provide relief.
If the SVT has occurred due to varicose veins, it is essential to treat the varicose veins preventively after the acute symptoms subside, in order to prevent a recurrence of superficial vein thrombosis.
A deep vein thrombosis (DVT) is a medical emergency. It involves the blockage of one or more deep leg or pelvic veins by a blood clot (thrombus), posing a life-threatening risk to the affected leg.
A deep vein thrombosis (DVT) can arise and be promoted by various causes
lack of movement due to bedridden conditions,
immobilization or fixation due to orthopedic diseases (splints/casts,
serious illnesses such as cancer,
long trips (flights, car rides),
genetic or acquired disorders of blood clotting and increased clotting tendency after surgeries, dehydration (lack of fluids), medications (e.g., hormone therapy such as birth control pills), chemotherapy,
injuries and trauma to the veins
What symptoms can a deep vein thrombosis cause?
Typical symptoms include pain in the calf, thigh, or hip, which worsens when walking and standing, depending on the location of the thrombosis.
Swelling, warmth, or reddish-blue skin discoloration can also be signs of a deep vein thrombosis.
Visible veins: When blood can no longer flow properly through the blocked vein, it may find alternative routes. It often flows more through veins located closer to the surface. These can protrude and become clearly visible as 'warning veins' on the shin.
How is a thrombosis diagnosed at the Vein Center at KuDamm?
The diagnosis of a deep vein thrombosis is made during an acute visit to our clinic through a clinical examination combined with a careful ultrasound examination and your individual medical history. In some cases, a D-dimer test is also conducted to determine the thrombosis markers in the blood.
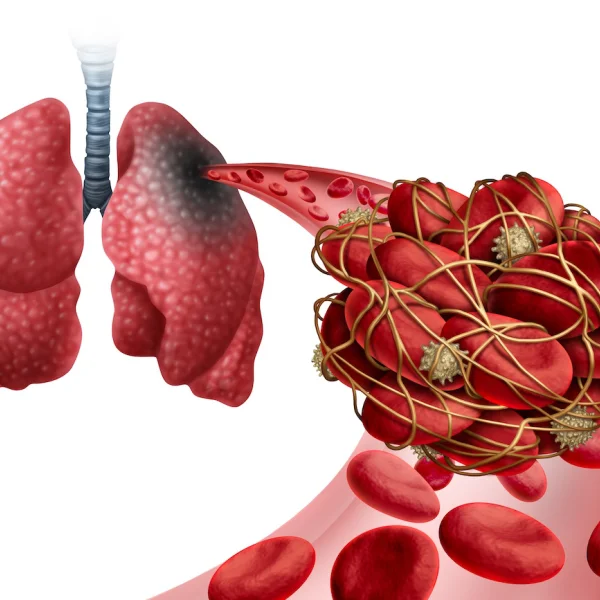
Dangerous complication: Pulmonary embolism
Especially in untreated leg and pelvic vein thromboses, there is a risk of a potentially life-threatening pulmonary embolism:
Parts of the thrombus can detach and be carried with the bloodstream into a vessel in the lungs.
Possible symptoms of a pulmonary artery embolism include sudden shortness of breath, chest pain, coughing, palpitations or rapid heartbeat, and loss of consciousness.
A large pulmonary embolism puts strain on the heart. In the worst case, it can lead to heart failure and can be life-threatening.
If you suspect a pulmonary embolism, go immediately to an emergency department or call emergency services.
The prompt initiation of consistent compression therapy in acute deep vein thrombosis is essential for the prevention of post-thrombotic syndrome.
Treatment of a deep vein thrombosis (DVT) at the Vein Center at KuDamm
The main goal is to prevent the growth of the blood clot, restore normal blood flow, and avoid life-threatening complications such as a pulmonary embolism.
The treatment of DVT should always be carried out and monitored by a specialist.
The therapy of choice is anticoagulation with a blood-thinning medication in tablet or injection form, and long-term compression therapy with custom-made compression stockings of class II to avoid post-thrombotic syndrome as much as possible.
Immediately, compression therapy should be initiated with a compression bandage if no appropriate stocking is available. Compression therapy relieves pain and discomfort, helps break down the thrombus through external pressure, and normalizes blood flow in the veins.
Local therapy of the affected areas through cooling, ointments (e.g., heparin), and anti-inflammatory pain relievers can also provide relief.
The long-term consequence of a deep vein thrombosis can be the so-called post-thrombotic syndrome. Depending on the diagnostic criteria, 20–63% of patients develop post-thrombotic syndrome (PTS) with a feeling of heaviness, tendency to swell, and pain, with varying stages of chronic venous insufficiency (CVI) up to trophic disorders and ulcerations (leg ulcers).
Special form: Muscle vein thrombosis
Muscle vein thrombosis is a distinct condition.
It usually occurs in the lower leg in the calf muscles.
The superficial calf muscles consist of the gastrocnemius muscle with its two parts, the medial head (caput mediale) and the lateral head (caput laterale). Below it lies the soleus muscle.
The development of a calf muscle vein thrombosis can have many causes.
Immobilizations such as long-haul flights, long car trips, surgeries followed by splinting/partial load of the leg, varicose veins, superficial vein thromboses, varicose vein surgeries, and sclerotherapy as part of a post-thrombotic syndrome.
What symptoms does a muscle vein thrombosis cause?
Many muscle vein thromboses go unnoticed, as the muscle veins are paired (there are always two), so that when one vein is blocked, the other can usually compensate for and take over the transport function.
In a symptomatic muscle vein thrombosis, there is usually localized pain in the area of the calf muscles that increases with movement.
The diagnosis is made through sonography using a high-resolution ultrasound device and by an experienced examiner.
How is a muscle vein thrombosis treated?
Diagnosis and treatment should always be performed if there is a suspicion of muscle vein thrombosis, to reduce complications such as thrombus growth into the deep leg veins, the risk of a pulmonary embolism, and the development of post-thrombotic syndrome.
According to current studies, in the case of an unnoticed muscle vein thrombosis, it is assumed that approximately 80% of isolated muscle vein thromboses will resolve on their own within three months.
If a muscle vein thrombosis is present, anticoagulation (blood thinning), typically for three months, should be initiated immediately, in combination with compression therapy using class II compression stockings, and closely monitored by a phlebologist.
FAQ on Thrombosis Diagnosis
Wie wird eine tiefe Venenthrombose behandelt?
Eine unbehandelte Thrombose kann möglicherweise lebensgefährliche Komplikation, wie eine Lungenembolie, zur Folge haben. Daher muss jeder klinische Thromboseverdacht rasch so weit abgeklärt werden, dass eine sichere Therapieentscheidung getroffen werden und eine Therapie eingeleitet werden kann.
Die Zielsetzung der Akutbehandlung einer tiefen Becken-/ Beinvenenthrombose besteht vorrangig darin, ein weiteres Wachstum des Thrombus zu verhindern und das Risiko von lebensbedrohlichen Komplikationen, wie das einer Lungenembolie, zu reduzieren.
Die Behandlung mit gerinnungshemmenden Medikamenten selbst bewirkt zwar keine Auflösung des Blutgerinnsels, hilft dem Organismus aber, die körpereigenen Mechanismen zur Auflösung des Thrombus anzukurbeln (Fibrinolyse).
Mit der zügigen Einleitung einer therapeutischen Antikoagulation sinkt das Risiko für eine erneute tiefe Venenthrombose und eine Lungenembolie. Eine frühzeitige begonnene Therapie reduziert auch das Auftreten und den Schweregrad eines postthrombotischen Syndroms.
Der aktuelle Standard der Thrombosetherapie besteht aus gerinnungshemmenden Medikamenten („Blutverdünner“). Diese können sowohl in Spitzenform, als auch in Tablettenform eingenommen werden. Zusätzlich sollte bei jeder Thrombose eine sofortige Kompressionstherapie der betroffenen Extremität (Bein, Arm) durch eine Kompressionsbadagierung oder einen Kompressionsstrumft nach Maß der Kompressionsklasse II erfolgen. Durch den Kompressionsdruck von außen wird der Blutfluss im Bein schneller normalisiert und der Schweregrad eines eventuell später auftretenden, postthrombotischen Syndroms wird reduziert.